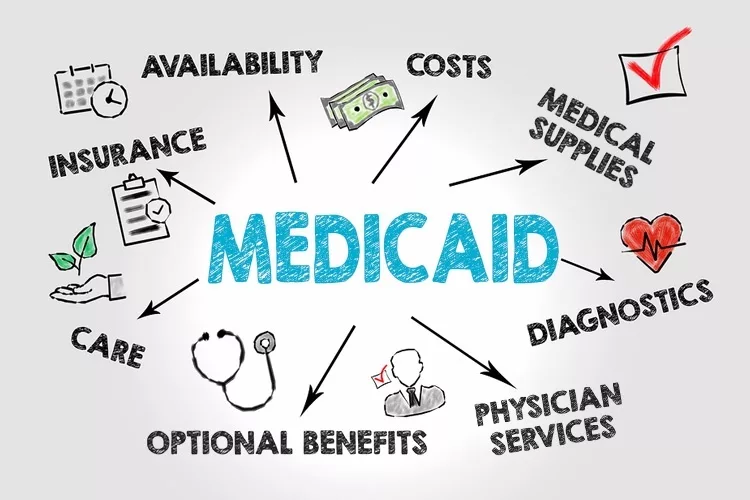
In the discourse surrounding healthcare, the allocation of resources to support the medical needs of low-income individuals has been a contentious issue. At the forefront of this discussion lies Medicaid, a program designed to extend healthcare coverage to those who cannot afford it. While the intention behind increasing federal funding for Medicaid may seem benevolent, the implications are far-reaching and warrant careful consideration.
Understanding Medicaid: A Vital Lifeline or an Economic Burden?
The Role of Medicaid in Healthcare Access
Medicaid stands as a crucial pillar in the American healthcare system, providing coverage to vulnerable populations such as children, pregnant women, elderly, and individuals with disabilities. The program serves as a safety net, ensuring that basic medical needs are met for those who lack the financial means to access healthcare services independently.
However, the debate over the expansion of Medicaid funding brings to light multifaceted concerns that extend beyond mere access to healthcare. While it is undeniable that healthcare is a fundamental human right, the manner in which it is financed and administered warrants scrutiny.
Federal Intervention vs. State Autonomy: Striking a Balance
The fundamental question at hand revolves around the appropriate level of government involvement in healthcare provision. Should the federal government increase funding for Medicaid, or should states be entrusted with the autonomy to tailor healthcare programs to their unique demographic and economic landscapes?
In advocating for state-level management of Medicaid programs, proponents argue for increased flexibility and accountability. States are better positioned to assess the needs of their populations and implement targeted interventions that address specific healthcare challenges. Moreover, decentralization fosters innovation and experimentation, allowing states to pioneer initiatives that could serve as models for effective healthcare delivery nationwide.
Conversely, proponents of federal intervention emphasize the need for standardized guidelines and equitable distribution of resources. They argue that a centralized approach ensures consistency and prevents discrepancies in healthcare access across state lines. Additionally, federal oversight is perceived as a safeguard against potential disparities in care quality and coverage.
Economic Ramifications of Escalating Medicaid Funding
Balancing Healthcare Access and Fiscal Responsibility
While the moral imperative to expand healthcare coverage is compelling, it is imperative to assess the economic implications of escalating Medicaid funding. The infusion of federal dollars into Medicaid may yield short-term gains in healthcare access, but the long-term ramifications on the economy cannot be overlooked.
Increased federal funding necessitates revenue generation through mechanisms such as taxation or government borrowing. Such measures, while intended to bolster healthcare accessibility, can inadvertently strain the economy and impede individual financial well-being. The European model serves as a cautionary tale, where exorbitant tax rates to fund universal healthcare have stymied economic growth and encroached upon individual financial freedom.
Efficiency vs. Dependency: The Perils of Overreliance on Federal Aid
An underexplored facet of the Medicaid debate pertains to the potential repercussions of heightened federal funding on state-level governance and fiscal responsibility. The prospect of receiving increased federal aid may inadvertently disincentivize states from implementing cost-effective measures and fostering fiscal discipline.
States may become reliant on federal subsidies, thereby relinquishing their autonomy and accountability in healthcare management. The absence of fiscal constraints could breed inefficiency and bureaucratic bloat within Medicaid programs, exacerbating budgetary pressures and impeding sustainable healthcare delivery.
Challenges and Ethical Dilemmas in Medicaid Administration
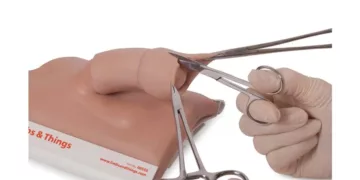
The Conundrum of Asset Disposal and Medicaid Eligibility
One of the most contentious issues surrounding Medicaid eligibility pertains to asset disposal and the treatment of individuals with property or assets. The dichotomy between healthcare access and asset retention underscores the ethical dilemmas inherent in Medicaid administration.
Individuals who require Medicaid assistance often find themselves compelled to liquidate assets, including real estate, to qualify for coverage. This requirement poses a significant burden on low-income individuals and underscores the inherent inequities within the healthcare system. Moreover, it perpetuates a cycle of financial instability and exacerbates socioeconomic disparities among vulnerable populations.
Mitigating Fraud and Abuse: Safeguarding Medicaid Integrity
A critical challenge in Medicaid administration lies in combating fraud and abuse, which undermine the integrity of the program and strain finite resources. Instances of individuals exploiting Medicaid benefits without genuine need highlight systemic vulnerabilities that warrant robust oversight and enforcement mechanisms.
Addressing fraud requires a multifaceted approach encompassing enhanced monitoring, data analytics, and collaboration between government agencies and healthcare providers. By leveraging technology and adopting proactive strategies, policymakers can mitigate fraudulent activities and preserve the sustainability of Medicaid for those truly in need.
Navigating the Complexities of Healthcare Policy
In conclusion, the debate surrounding Medicaid funding epitomizes the intricate interplay between healthcare access, fiscal responsibility, and ethical imperatives. While the imperative to ensure universal healthcare coverage is indisputable, the means by which it is achieved necessitates nuanced deliberation and principled decision-making.
Rather than advocating for indiscriminate escalation of federal funding, policymakers must prioritize holistic solutions that reconcile healthcare accessibility with economic sustainability. Empowering states to innovate and tailor Medicaid programs to local needs while safeguarding against fiscal irresponsibility is paramount in fostering a resilient and equitable healthcare system.
As we navigate the complexities of healthcare policy, let us remain steadfast in our commitment to upholding the principles of fairness, efficiency, and compassion in serving the healthcare needs of all Americans.
“Healthcare is a human right, but its provision demands a delicate balance of fiscal prudence and ethical stewardship.” – Anonymous
By embracing collaboration, innovation, and empathy, we can forge a path towards a healthcare system that is not only accessible but also sustainable for generations to come.
For more content, check out The Imperative Dilemma: Requiring Work for Medicaid Eligibility.
Additional Resources:
- The European Model: Lessons for U.S. Healthcare Reform
- Medicaid Fraud and Abuse: Challenges and Solutions
- State Innovation in Medicaid Administration: Best Practices and Case Studies
In crafting a coherent healthcare policy, it is imperative that we engage in informed discourse, drawing upon diverse perspectives and empirical evidence to inform our decision-making. Together, let us embark on a journey towards a healthier, more equitable future for all.
Note: The views expressed in this blog post are the author’s personal opinions.